Molecular Nociception Group
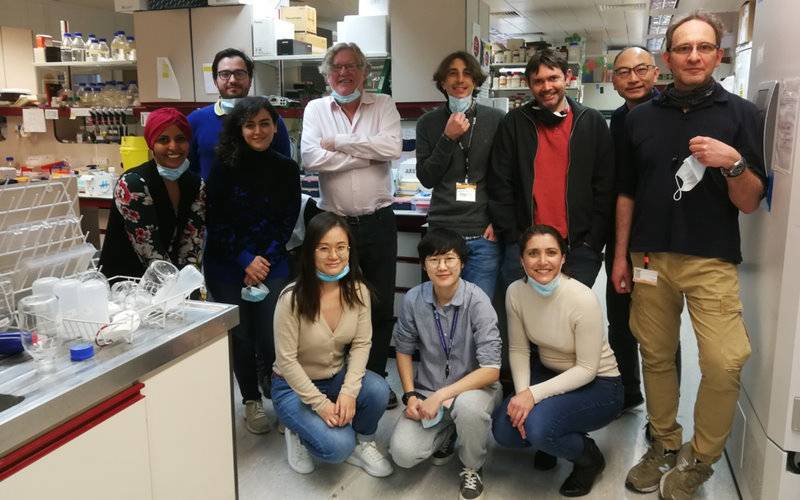
 James J Cox PhD, John N Wood FRS, Jing Zhao MD PhD
James J Cox PhD, John N Wood FRS, Jing Zhao MD PhD

Our research
The twenty-first century has seen a revolution in our understanding of the receptor systems and regulatory pathways that underlie the responses of nociceptors to the occurrence of tissue damage. This has important implications for human health and disease.
We collaborate with research groups in Europe, the United States, Korea, Japan, and Australia, using transgenic mouse models, natural products, and cloned genes to explore the physiology of pain perception. The systems we study have a broad relevance to understanding how the nervous system works in terms of synaptic plasticity, responses to environmental stimuli, sensation, and behaviour.
Lab Manager
Sam Gossage
Recent Post-Doctoral Fellows
- Sascha R.A. Alles PhD
- Ali Bangash MD PhD
- Shafaq Sikandar PhD
- Ana Luiz PhD
- Edward C. Emery PhD
- John Linley PhD
- Naxi Tian PhD
- Manuel Arcangeletti PhD
- Federico Iseppon PhD
Recent PhD Students
- 2014 Sam Shepherd
- 2014 Alexandros Kanellopoulos
- 2015 Man-Cheung Lee
- 2015 Jenny Koenig
- 2015 Shengnan Li
- 2016 Sonia Santana-Varela
- 2019 Larissa de Clauser
- 2020 Donald MacDonald
- 2020 Alice Fuller
- 2023 Rayan Haroun
- 2023 Clarissa Butti
Selected publications
Embracing cancer complexity: Hallmarks of systemic disease. Swanton C, Bernard E, Abbosh C, André F, Auwerx J, Balmain A, Bar-Sagi D, Bernards R, Bullman S, DeGregori J, Elliott C, Erez A, Evan G, Febbraio MA, Hidalgo A, Jamal-Hanjani M, Joyce JA, Kaiser M, Lamia K, Locasale JW, Loi S, Malanchi I, Merad M, Musgrave K, Patel KJ, Quezada S, Wargo JA, Weeraratna A, White E, Winkler F, Wood JN, Vousden KH, Hanahan D. Cell. 2024 Mar 28;187(7):1589-1616
Tentonin 3 is a pore-forming subunit of a slow inactivation mechanosensitive channel. Pak S, Ryu H, Lim S, Nguyen TL, Yang S, Kang S, Yu YG, Woo J, Kim C, Fenollar-Ferrer C, Wood JN, Lee MO, Hong GS, Han K, Kim TS, Oh U. Cell Rep. 2024 Jun 7;43(6):114334.
Genetic landscape of congenital insensitivity to pain and hereditary sensory and autonomic neuropathies. Lischka A, Eggermann K, Record CJ, Dohrn MF, Laššuthová P, Kraft F, Begemann M, Dey D, Eggermann T, Beijer D, Šoukalová J, Laura M, Rossor AM, Mazanec R, Van Lent J, Tomaselli PJ, Ungelenk M, Debus KY, Feely SME, Gläser D, Jagadeesh S, Martin M, Govindaraj GM, Singhi P, Baineni R, Biswal N, Ibarra-Ramírez M, Bonduelle M, Gess B, Romero Sánchez J, Suthar R, Udani V, Nalini A, Unnikrishnan G, Marques W Junior, Mercier S, Procaccio V, Bris C, Suresh B, Reddy V, Skorupinska M, Bonello-Palot N, Mochel F, Dahl G, Sasidharan K, Devassikutty FM, Nampoothiri S, Rodovalho Doriqui MJ, Müller-Felber W, Vill K, Haack TB, Dufke A, Abele M, Stucka R, Siddiqi S, Ullah N, Spranger S, Chiabrando D, Bolgül BS, Parman Y, Seeman P, Lampert A, Schulz JB, Wood JN, Cox JJ, Auer-Grumbach M, Timmerman V, de Winter J, Themistocleous AC, Shy M, Bennett DL, Baets J, Hübner CA, Leipold E, Züchner S, Elbracht M, Çakar A, Senderek J, Hornemann T, Woods CG, Reilly MM, Kurth I. Brain. 2023 Dec 1;146(12):4880-4890.
Chemogenetic Silencing of NaV1.8-Positive Sensory Neurons Reverses Chronic Neuropathic and Bone Cancer Pain in FLEx PSAM4-GlyR Mice. Haroun R, Gossage SJ, Luiz AP, Arcangeletti M, Sikandar S, Zhao J, Cox JJ, Wood JN. eNeuro. 2023 Sep 26;10(9):ENEURO.0151-23.2023.
Gate control of sensory neurotransmission in peripheral ganglia by proprioceptive sensory neurons. Fuller AM, Luiz A, Tian N, Arcangeletti M, Iseppon F, Sexton JE, Millet Q, Caxaria S, Ketabi N, Celik P, Wood JN, Sikandar S. Brain. 2023 Oct 3;146(10):4033-4039.
Molecular basis of FAAH-OUT-associated human pain insensitivity. Mikaeili H, Habib AM, Yeung CW, Santana-Varela S, Luiz AP, Panteleeva K, Zuberi S, Athanasiou-Fragkouli A, Houlden H, Wood JN, Okorokov AL, Cox JJ. Brain. 2023 Sep 1;146(9):3851-3865.
Neutrophils infiltrate sensory ganglia and mediate chronic widespread pain in fibromyalgia. Caxaria S, Bharde S, Fuller AM, Evans R, Thomas B, Celik P, Dell'Accio F, Yona S, Gilroy D, Voisin MB, Wood JN, Sikandar S. Proc Natl Acad Sci U S A. 2023 Apr 25;120(17):e2211631120
Pregabalin Silences Oxaliplatin-Activated Sensory Neurons to Relieve Cold Allodynia. Iseppon F, Luiz AP, Linley JE, Wood JN. eNeuro. 2023 Feb 21;10(2):ENEURO.0395-22.2022
Transcriptomic and proteomic profiling of NaV1.8-expressing mouse nociceptors. Schmidt M, Sondermann JR, Gomez-Varela D, Çubuk C, Millet Q, Lewis MJ, Wood JN, Zhao J. Front Mol Neurosci. 2022 Oct 11;15:1002842.
Genetic pain loss disorders. Lischka A, Lassuthova P, Çakar A, Record CJ, Van Lent J, Baets J, Dohrn MF, Senderek J, Lampert A, Bennett DL, Wood JN, Timmerman V, Hornemann T, Auer-Grumbach M, Parman Y, Hübner CA, Elbracht M, Eggermann K, Geoffrey Woods C, Cox JJ, Reilly MM, Kurth I. Nat Rev Dis Primers. 2022 Jun 16;8(1):41
A central mechanism of analgesia in mice and humans lacking the sodium channel NaV1.7. MacDonald DI, Sikandar S, Weiss J, Pyrski M, Luiz AP, Millet Q, Emery EC, Mancini F, Iannetti GD, Alles SRA, Arcangeletti M, Zhao J, Cox JJ, Brownstone RM, Zufall F, Wood JN. Neuron. 2021 May 5;109(9):1497-1512
Silent cold-sensing neurons contribute to cold allodynia in neuropathic pain. MacDonald DI, Luiz AP, Iseppon F, Millet Q, Emery EC, Wood JN. Brain. 2021 Jul 28;144(6):1711-1726
Facilities
Related programmes
Researchers within the Wolfson Institute for Biomedical Research contribute to several distinguished taught courses at UCL.
Group activities




 Close
Close