Best disease is the most common of the bestrophinopathies.
What is Best disease?
Best vitelliform macular dystrophy (BVMD), more commonly known as Best Disease is the most common bestrophinopathy, affecting the retinal pigment epithelium (RPE) cells at the back of the eye. The first case of Best disease was first discovered by clinicians at Moorfields Eye Hospital, but it was named after the German ophthalmologist, Dr. Friedrich Best, who examined a large family with this condition in the early 1900’s. Best disease is categorized by the appearance of a vitelliform lesion (Latin for ‘egg-yolk’) on the macula, this is usually bilateral, meaning this yellow ‘egg-yolk’ appearance of the macula is present in both eyes of the affected individual. Best disease follows a dominant mode of inheritance and can display incomplete penetrance and variable expressivity, therefore even though it is a disease which is passed down genetically, there can be differences amongst those affected with Best’s, even within the same family.
Best Disease usually occurs in childhood, the ‘egg-yolk’ lesion is mostly seen between the ages of 3 to 15 years of age. There have been many studies into how common Best disease is within different populations, it is thought to affect between 1 and 9 out of every 100,000 people. Adult onset versions of Best disease are categorised and termed Adult vitelliform Macular Degeneration.
How does Best disease affect the eye?
Best disease is thought to progress through a number of distinct stages:
Stage I – Previtelliform stage - Vision at this early stage of Bests is normal and can be as good as 6/6 on a Snellen chart. Previtelliform means that it is before the classic yellow ‘egg-yolk’ lesion formation. The RPE may be normal or there could be very subtle changes such as small structures which resemble honeycombs being present. These may appear on the retina as yellowish pigment changes centrally.
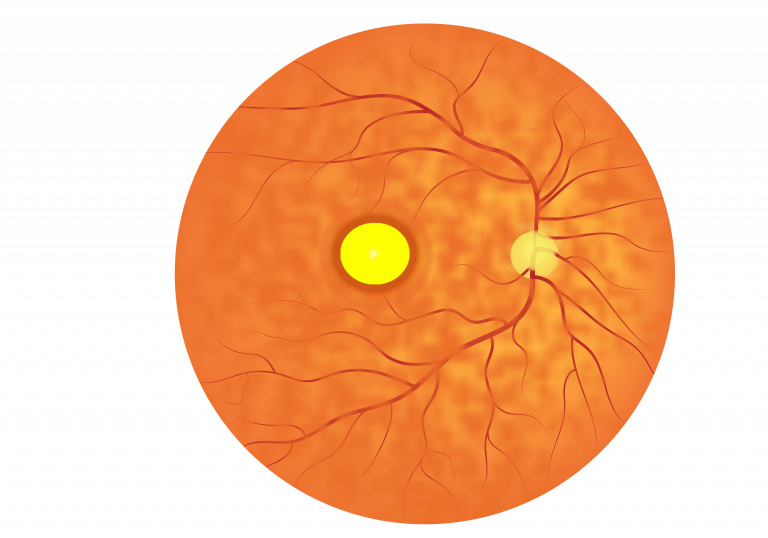
- Stage II – Vitelliform stage – There may be mild vision loss in this stage of disease or vision could be normal. The vitelliform stage is the classic stage in which Bests is most easily identified, by the presence of a yellow ‘egg-yolk’ like lesion on the macula which is usually 2-3 mm in diameter.
- Stage III – Pseudohypopyon stage – There may be mild vision loss in this stage of disease. The build up of fatty deposits, termed lipofuscin, can lead to the formation of pseudohypopyon, where cells involved in inflammation build up in the anterior chamber of the eye.
Stage IV – Vitelleruptive stage – Vision will be similar to earlier stages or even be mildly decreased from previous stages. At stage IV, the “egg-yolk” lesions breaks up leading to a lesion resembling a ‘scrambled-egg’. Irregular yellow deposits can also be observed at the back of the eye’
Stage V – Atrophic stage – Vision will be greatly reduced at this stage, classically vision can range from 6/12 on a Snellen chart to 6/60 or less. Death of the RPE in the macular region can lead to the cell loss of retinal cells, including the photoreceptor cells crucial for normal vision. Scar tissue forms at the back of the eye.
Stage VI – Choroidal neovascularization (CNV) stage – Vision in this stage is often 6/60 or even worse. This CNV stage occurs in around 1 in 5 patients suffering from Best disease. CNV is the growth of new blood vessels from the choroidal blood supply at the back of the eye. The RPE forms a barrier between the retina and the blood supply. When the RPE cells are lost from the macular region, new blood vessels can grow in from the choroid to the retina. Often, these new blood vessels are very weak and may even break and leak, causing the build-up of fluid in the retina. A sudden change in vision could indicate CNV, which can be treated using photodynamic therapy, laser treatment or through injections of VEGF therapy.
Loss of vision in Bests disease can be slow and gradual, or can occur rapidly, and progression through the disease stages can vary in individuals and families. Many patients report problems with reading small print (long-sighted) and may have astigmatism (a ‘rugby ball’ shape eye). One in four patients may also have multiple lesions in the retina and some of these may be away from the macula. The image below is a schematic of a fundus which is characteristic of a patient with Best Disease:
How is Best disease diagnosed?
Best disease can be diagnosed by looking for the characteristic egg-yolk-like lesions at the back of the eye observed in the vitelliform stage. Other tests are available to confirm the diagnosis.
OCT can be used to localize the lesion and look at its thickness, this may reveal elevation of the RPE with build-up of both lipofuscin and fluid.
The build-up of fatty deposits at the back of the eye can be detected using autofluorescent imaging. Autofluorescence can increase during early stages of disease.
An electrophysiological test, known as an EOG can be used to detect Best disease in patients. The EOG test is used to assess the activity and health of the RPE cells at the back of the eye. The test is used to calculate the Arden ratio, typically patients with Best disease have a ratio of 1.5 or lower, however EOG recordings in some patients can be normal. ERG tests, which measure retinal function, are normal in Best disease patients.
Best disease can be confirmed by genetic testing.
Are there any complications of Best disease?
Complications of Best disease generally occur during the late, atrophic stages of disease, and can lead to a rapid deterioration of vision.
Geographic Atrophy
Late stage disease is associated with the formation of scar tissue as the RPE cells at the back of the eye degenerate. Death of the RPE causes more widespread death of the retinal photoreceptor cells, termed geographic atrophy, leading to progressive and irreversible loss of vision.
Choroidal neovascularization (CNV)
The loss of RPE cells during late stage disease can lead to the formation of new blood vessels from the choroid to the retina. These new vessels can be weak, and rupture easily, leading to leakage and the build-up of fluid under the retina, greatly reducing vision. These bleeds can occur with only modest trauma.
Macular hole
The formation of a macular hole is a rare complication of Best disease. A macular hole is a tear in the macular region, which can result in a sudden decrease in vision in one eye.
What are the treatment options for Best disease?
There are currently no medical or surgical treatment options available for Best disease, or any of the bestrophinopathies. Scientists are currently developing new treatments and research is ongoing
Treatments are available for the complications of Best disease
Long-sightedness (hyperopia)
Hyperopia and astigmatism can be corrected using prescription glasses and contact lenses.
Choroid neovascularisation (CNV)
CNV can be treated by injecting anti-VEGF drugs (e.g. Avastin, Bevacizumab) into the back of the eye in an eye clinic. These injections can stop the growth of newer vessels, with the aim to preserve vision. CNV can also be treated using photodynamic therapy or laser therapy to shrink or seal the leaky blood vessels.
Macular holes
Macular holes can be treated in a surgical procedure.
Research into treatments for Best disease is ongoing. Patients are encouraged to visit the many charities and support groups for bestrophinopathies.
 Close
Close

