Lung cancer research: Insights into preclinical models
31 May 2024
Laboratory models of tumours are widely used and valuable tools for cancer research. However, there are limitations to how well these models can represent the genetic complexity of primary tumours.
As a result of scientific advances, it is increasingly possible to study cancer cells from patients directly in the laboratory. This can be achieved in a dish, as cell cultures or ‘organoids’, or in mouse models. For many applications it is vital that the laboratory models accurately reflect the complexity of the patient’s tumour, but how much of this complexity is maintained is unclear. In a new study by Professor Charles Swanton’s team at UCL and the Francis Crick Institute, researchers looked for some answers.
The study, published in Nature Communications, found that non-small cell lung cancer (NSCLC) tissue samples changed genetically when grown in mice for research, highlighting the need for further understanding of PDX model genomics if they are to be used clinically in the future.
Patient-derived xenograft (PDX) models are specialised models used in cancer research. Following surgery to remove the tumour, tumour cells from a patient are implanted into mice where they continue to grow. These models are a highly useful research tool as they can mimic how tumours grow and respond to treatment in the human body more accurately and efficiently than other types of laboratory models. This has led to the use of PDX models in pre-clinical drug testing and as ‘avatars’ in personalized medicine approaches.
However, these types of models do have limitations. For example, they do not completely mimic every aspect of how tumours develop and interact with other systems – such as the immune system. Also, they can accumulate new genetic changes as they grow in mice, so they no longer match up with original tumour cells from patients.
"There's currently no consensus about the degree of genetic changes that happen in PDX models. So, it was important to examine how accurately these models reflect real tumours and their spread to other parts of the body,” says Dr Rob Hynds, Senior Research Fellow (UCL Cancer Institute and UCL Great Ormond Street Institute of Child Health) and co-lead author* of the study.
“We used samples from patients enrolled in Cancer Research UK’s TRACERx study to create non-small cell lung cancer PDX models and monitored the genetic changes as we established and grew the models. We found there was a loss of genetic diversity – a ‘genetic bottleneck’ – where only a subset of the tumour cells survived and grew in the mice, causing differences between the original tumour and the mouse model.”
PDX models will remain a crucial tool for studying cancer before human clinical trials, both for NSCLC and other types of tumours, but further investigation is needed to make these models even more useful in the future.
"When using PDX models for research, we have to be mindful of the genetic changes that can occur. PDX models are ideal for certain types of studies, but we also need to consider their limitations, especially when considering them for use in the development of personalized treatments for patients or to predict pathways to therapy resistance, where it is vital that we are able to consider the response of the whole tumour,” says Dr Hynds.
* Additional co-lead authors: Dr Ariana Huebner and Dr David Pearce
Further information
- Research Paper: Representation of genomic intratumor heterogeneity in multi-region non-small cell lung cancer patient-derived xenograft models. Nature Communications
- Comment: Capturing heterogeneity in PDX models: representation matters. Nature Communications
- Dr Rob Hynds academic profile
- Swanton lab: Cancer Evolution and Genome Instability Laboratory
- UCL Cancer Institute
- UCL Great Ormond Street Institute of Child Health
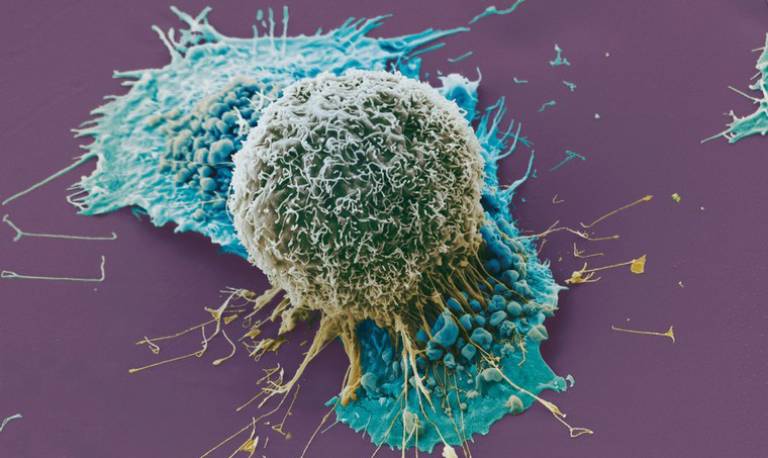
Main Image: Lung Cancer cells grown in culture, SEM. Anne Weston, Francis Crick Institute. Wellcome Images
 Close
Close

