There are no treatments that have been proven to slow the neurodegenerative process of Parkinson's disease despite encouraging findings in laboratory models of the disease.
In April 2016, one of the first studies to be initiated at the Leonard Wolfson Experimental Neurology Centre CRF was completed following recruitment and 60 weeks follow up of 60 participants in less than two years. The 'Exenatide-PD' study, a Phase II, double-blinded trial in Parkinson's disease funded by the Michael J Fox Foundation, and sponsored by UCL, investigated the potential neuroprotective properties of Exenatide, a drug licensed for the treatment of type 2 diabetes. The trial was led by Professor Tom Foltynie (Chief Investigator) based at the UCL Institute of Neurology.
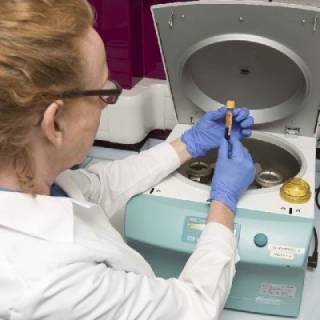
Prior work with exenatide demonstrated that as well as having positive effects on blood glucose, it stimulates GLP1 receptors in the brain triggering a cascade of pro-survival proteins including Akt. In an earlier small, open label proof of concept trial exenatide was shown to have benefits on the motor and cognitive deficits in Parkinson's disease in comparison to controls, that persisted for a year after cessation of the drug. Based on this, and using the new LWENC CRF, 60 patients with Parkinson's disease were assessed every three months while injecting either the active drug/matched placebo subcutaneously once weekly for a year, and again after having stopped injecting for a further three months. This represented the first randomised, placebo-controlled trial of exenatide as a potential disease modifying agent in Parkinson's disease.
Clinical, imaging and biomarker data has now been compared between those patients exposed to active drug in comparison to placebo, and results have been accepted for publication in The Lancet, replicating the positive trial results previously seen. Patients randomised to inject exenatide for one year had a statistically significant improvement in the severity of the motor aspects of their Parkinson's disease compared to patients randomised to inject placebo. These results are being explored further to identify the characteristics of patients (clinical phenotypes, genotypes and serum biomarkers) that are associated with the greatest responses to exenatide.
 Close
Close

